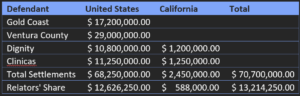
August 23, 2022. The United States Department of Justice settled three cases against a California county organized health system and three healthcare providers for alleged submission of false claims to California’s Medicaid program (Medi-Cal). Under the terms of the settlements, the county organized health system (COHS), an integrated health care system, a non-profit hospital system, and another non-profit healthcare organization paid a combined total of approximately $70 million. The former controller and former director of member services of the COHS, Gold Coast Health Plan, blew the whistle on the organization’s practices. Under the qui tam provision of the False Claims Act, which allows private citizens to sue on behalf of the government, the whistleblowers are entitled to a share of the government’s recovery. They also made claims under California’s state False Claims Act (CFCA). For reporting Medicaid fraud, the whistleblowers, or relators, will receive 18.5 percent of the federal government’s recovery and 24% of California’s recovery.
Ventura County Medi-Cal Managed Care Commission d/b/a Gold Coast Health Plan manages the “provision of health care services under California’s Medicaid program (Medi-Cal) in Ventura County, California.” The Affordable Care Act permitted states to expand Medicaid to cover “adults with incomes up to 138% of the Federal Poverty Level […] and provided states with an enhanced federal matching rate (FMAP) for their expansion populations.” California implemented Medicaid expansion in January 2014, which over time resulted in a 58% reduction in the uninsured rate from 2010-2019. California COHS organizations were required to return any unused funds if they did not spend at least 85% of their funding on “allowed medical expenses.” As Medicaid is both state and federally funded, California was then supposed to return those unused funds to the federal government.
According to the allegations, Ventura County, Gold Coast, and the two non-profit healthcare systems—Dignity Health (Dignity Health) and Clinicas del Camino Real Inc. (Clinicas)—submitted false claims to Medicaid so as to boost their spend to meet the 85% mark and not have to return any funds to the state. Gold Coast created Memorandums of Understanding (MOU) with Clinicas, Dignity Health, and Ventura County to encompass “Additional Services provided” to Adult Expansion Medi-Cal members. The relators alleged that the payments under these MOU were not for medically necessary services and further that the payments for Adult Expansion Medi-Cal members were “unlawful gifts of public funds” in violation of California law. The defendants denied the allegations.
Medicaid expansion presented the opportunity for people living on the edge of poverty to obtain healthcare coverage, particularly after the ACA’s individual mandate made not having healthcare costly, in the form of a monthly penalty for each month a person did not have health insurance (prior to 2019). As the Principal Deputy Assistant Attorney General said about this case, “Federal health care funds are not intended to serve as a blank check.” The Acting U.S. Attorney for the Central District of California added, “The money at issue in this case was designated by the federal government to pay for services to treat Medicaid expansion patients, and it never should have been used to double-pay for services that already had been reimbursed or to pay for services that simply were never provided.”
The whistleblowers who called out this misconduct were rewarded approximately $13 million plus attorneys’ fees. The Department of Justice and state health departments need whistleblowers to report fraud against Medicaid in hospitals, healthcare providers, and county health programs.
If you would like to report Medicaid fraud, you can contact the California whistleblower attorneys at Tycko & Zavareei LLP. Eva Gunasekera and Renée Brooker are former officials of the United States Department of Justice and prosecuted whistleblower cases under the False Claims Act. Eva was the Senior Counsel for Health Care Fraud. Renée served as Assistant Director at the United States Department of Justice, the office that supervises False Claims Act cases in all 94 United States District Courts. Eva and Renée now represent whistleblowers. For a free consultation, you can contact Eva Gunasekera at eva@tzlegal.com or contact Renée at reneebrooker@tzlegal.com (tel.: 202-417-3664). Visit Tycko & Zavareei LLP’s website for whistleblowers to learn more at https://www.fraudfighters.net/.